This excerpt is from my book, "The Chlorine Dioxide Miracle: Safeguarding Health with Safe and Effective Applications." If you're interested in chlorine dioxide therapy, you can purchase the book here:
16.1 A Deeper Understanding of Cancer Treatment
Cancer refers to a disease where cells in the body lose control over their normal growth and division, continuously multiplying to form tumors. Solid tumors are those that arise from the abnormal proliferation of cells in specific organs, as opposed to hematologic tumors like leukemia. Solid tumors can be benign or malignant, with the latter being cancerous. Malignant solid tumors are invasive, breaching the boundaries of their original tissues, spreading to surrounding areas, and metastasizing to other parts of the body through the blood or lymphatic systems.
Cancer can be caused by various factors, including genetics, environmental exposures (like smoking, chemicals, and radiation), lifestyle choices (such as diet, weight, and exercise), and infections (from certain viruses and bacteria, for instance). The development of cancer can span many years, starting from normal cells to precancerous lesions, and ultimately to malignant tumors.
There are multiple treatment options for cancer, including surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. Surgery is commonly used to remove localized tumors. Radiation and chemotherapy aim to kill or halt the growth of cancer cells. Targeted therapy and immunotherapy are relatively newer treatments that leverage our understanding of the biological characteristics of cancer cells.
However, current treatments have several drawbacks. Surgery can remove tumors but is often ineffective against metastasized cancer. It carries high risks, causes significant trauma to the patient's body, requires a long recovery period, and may miss tiny cancer cells, leading to recurrence. Radiation and chemotherapy can target cancer cells throughout the body but are imprecise and toxic to normal cells, causing side effects like nausea, vomiting, hair loss, and immunosuppression. Due to the heterogeneity and adaptability of cancer cells, chemotherapy may not eradicate all cancer cells, and drug resistance can develop, reducing the effectiveness over time.
Targeted therapy and immunotherapy represent advancements in cancer treatment, offering more precise targeting of cancer cells or modulating the immune system to recognize and destroy them. However, targeted therapies only work on specific molecular targets, necessitating the expression of these targets on cancer cells. Cancer cells may lose these targets due to genetic mutations, leading to treatment failure. Immunotherapy has shown remarkable results in certain cancers, but not all patients respond, and it can sometimes trigger excessive immune responses that damage healthy tissue.
Both targeted therapy and immunotherapy are important modern cancer treatments, but they both have significant issues with resistance. Targeted therapy inhibits the growth and spread of cancer cells by focusing on unique molecular markers and signaling pathways, while immunotherapy aims to activate or boost the patient's immune system to identify and eliminate cancer cells.
Resistance to targeted therapy typically develops during treatment, as cancer cells evade the effects of drugs through genetic mutations or changes in expression. For instance, some drugs work by binding to specific proteins on the surface of cancer cells. However, cancer cells may alter the structure of these proteins to reduce drug binding or activate alternative growth signaling pathways to sustain their growth. Additionally, drug pumps within cancer cells can be activated to expel drugs from the cell, reducing the effective drug concentration. Due to these mechanisms, cancer cells can survive under treatment pressure, potentially leading to disease relapse or progression.
Immunotherapy resistance involves the complex interplay between cancer cells and the immune system. Cancer cells can evade immune surveillance through various mechanisms, such as expressing inhibitory molecules like PD-L1 to suppress T cell activity. Immunotherapies, like PD-1 or PD-L1 inhibitors, aim to block these inhibitory signals, but cancer cells may adapt by increasing other immune suppressive pathways. Moreover, other cells in the cancer cell microenvironment, such as regulatory T cells and tumor-associated macrophages, may counteract the tumor immune response, further promoting the development of resistance.
Although targeted therapy and immunotherapy have achieved some clinical success, the development of resistance remains a significant challenge. Due to the inevitable resistance, even these latest cancer treatment methods cannot be used repeatedly to treat cancer, and in the long term, they seem fleeting and unable to defeat cancer.
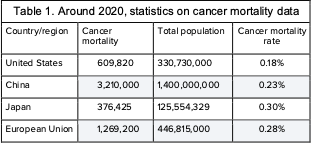
On the other hand, as can be seen from the table below, regions with much better cancer treatment conditions than China do not show a significantly lower cancer mortality rate compared to China, suggesting that modern cancer treatment methods have a limited effect during the fight against cancer (Table 1).
To evaluate the effectiveness of a cancer treatment method, we need to consider five key dimensions: convenience, safety, inhibition rate, drug resistance, and treatment sustainability. For example, oral chemotherapy drugs are relatively convenient to use but perform poorly in terms of safety, inhibition effect, and drug resistance. On the other hand, surgical treatment shows excellent results in inhibition and drug resistance, but its convenience and sustainability are lower due to the inability to be repeated frequently. Radiation therapy scores low in convenience and safety but has moderate inhibition effect, drug resistance, and good sustainability, making it suitable for cancer treatment at various stages. Targeted drugs and immune checkpoint inhibitors face challenges in drug resistance and sustainability. Although they can extend patients' survival for a period of time, many patients may still unfortunately pass away in the end.
An ideal cancer treatment should score high in all five aspects, which would potentially transform cancer into a chronic disease or even achieve its ultimate cure. Currently, the major cancer treatment methods do not score high in all these five dimensions. To improve the scores in each aspect, modern medical technology often focuses on a few dimensions. For example, directly injecting chemotherapy drugs or immunotherapy drugs into the tumor can significantly improve the scores in safety and inhibition rate at the expense of convenience.
16.2 Research on Chlorine Dioxide Treatment for Cancer[1]
[1] This section is mainly derived from my paper:https://doi.org/10.1101/2023.11.24.568512
I. Research Summary
Our team is currently investigating the use of chlorine dioxide for cancer treatment. Chlorine dioxide shares similar properties with powerful oxidizing agents known as ROS, which have been shown to destroy cancer cells and aid in tissue repair. We have discovered that chlorine dioxide can be safely used as a therapeutic agent in humans. Our research focuses on delivering chlorine dioxide directly into tumors as an innovative approach to cancer treatment. By targeting the tumor directly, chlorine dioxide can specifically kill cancer cells without promoting drug resistance. Additionally, chlorine dioxide has demonstrated the ability to stimulate an immune response against cancer, further enhancing its therapeutic effects. Our goal is to extend the lives of patients and transform cancer into a manageable chronic illness by injecting chlorine dioxide directly into tumors. This groundbreaking treatment utilizes the ROS-mimicking abilities of chlorine dioxide to eliminate cancer cells and promote tissue regeneration. By harnessing the unique properties of chlorine dioxide, we offer a new pathway to improve patient outcomes in cancer treatment. Ongoing studies are necessary to refine the delivery methods and dosage of chlorine dioxide, as well as explore its combined effects with other treatments. As research progresses, direct tumor injection of chlorine dioxide emerges as an exciting and promising approach to effective cancer therapy.
II. Introduction to the Research
Certain natural compounds or drugs that target Superoxide dismutase (SOD) have an incredible ability to selectively kill cancer cells by increasing the production or accumulation of ROS. Additionally, the body's own neutrophils can generate ROS, which aids in the destruction of cancer cells. Some drugs are designed specifically to elevate ROS levels within cancer cells, resulting in sustained suppression of the disease. For example, the combination of metformin, which raises ROS levels, and apigenin, which enhances this effect, exhibits a potent anticancer action while sparing healthy cells. Photodynamic therapy (PDT) is another technique that utilizes light to activate a photosensitizer drug in the body, generating singlet oxygen (1O2). This sudden surge of oxygen induces toxicity in tumor cells, leading to their death through apoptosis or necrosis. PDT not only directly targets and kills the tumor but also stimulates dendritic cells to release cell death-associated molecular patterns (DAMPs), initiating an immune response that targets antigens and promotes an anti-tumor immune reaction.
Building on this concept, our hypothesis suggests that the external addition of ROS or similar compounds could effectively destroy tumors and, similar to PDT, trigger an antitumor immune response. In this context, we have chosen chlorine dioxide as a ROS-mimicking oxidant to evaluate its potential in cancer treatment. chlorine dioxide, denoted by its chemical formula ClO2, is a powerful oxidizing agent with disinfectant properties. Its applications span various fields, including water purification, food sanitation, medical sterilization, and environmental decontamination. chlorine dioxide efficiently breaks down the cell membranes and DNA of bacteria, viruses, and other microbes, effectively eliminating pathogens and impurities. Notably, at a low concentration of 0.25 mg/L, chlorine dioxide can eliminate 99% of E. coli (15,000 cells/mL) within just 15 seconds. Furthermore, research has demonstrated that chlorine dioxide and hydrogen peroxide have similar efficacy in inducing cell death in human gingival fibroblasts.
ROS are generated during cellular respiration for ATP synthesis. However, the widespread production of ROS in the body and the limited capacity to rapidly eliminate a significant number of cells, particularly within tumor tissues, present significant challenges. These obstacles are primarily attributed to tumor hypoxia, characterized by low oxygen levels in the tumor environment. To establish a new standard for cancer treatment, it is crucial to increase the concentration of chlorine dioxide to a level where it can effectively eradicate large tumor masses, surpassing the body's natural production of ROS. Additionally, due to the short lifespan of chlorine dioxide as an oxidizing agent in body tissues and the need to minimize systemic side effects, we have chosen intratumoral administration of chlorine dioxide as the most effective method to achieve our goal.
III. Research Results and Discussion
This research explored the impact of a compound called chlorine dioxide on tumors and tissues, using mice as subjects. The findings revealed intriguing outcomes. chlorine dioxide exhibited toxicity towards both cancer cells and normal cells, without specific targeting. When injected beneath the mice's skin, it caused significant damage to the skin. However, within approximately 20 days, the damaged tissue fully healed, returning to its normal state and regrowing hair. This suggests that although chlorine dioxide may harm tissues, the body possesses the ability to repair itself.
To investigate wound healing, cuts were made on the mice's tails. Mice treated with chlorine dioxide or hydrogen peroxide experienced accelerated wound closure compared to those treated with saline solution alone. The wounds healed approximately 6 days earlier. Chlorine dioxide appeared to aid in the removal of dead tissue debris near the wounds, potentially contributing to the healing process.
Furthermore, direct injection of chlorine dioxide into tumors in mice resulted in significant inhibition of tumor growth. The tumors decreased in size, and signs of dead tissue within the tumors were observed. Additionally, chlorine dioxide administration significantly reduced the spread of cancer to the lungs.
The researchers proposed two mechanisms by which chlorine dioxide operates. Firstly, it induces cancer cell death through apoptosis (programmed cell death) or necrosis (uncontrolled cell death). Secondly, this cell death triggers an immune response against the tumor. When the immune system detects dead tumor cells, it recognizes the presence of cancer and initiates an attack.
Although injecting chlorine dioxide into tumors provided a short-term boost to the immune system against cancer, this effect was not sustained in the long term. In fact, chlorine dioxide may potentially weaken immune responses over time by increasing certain immune-suppressing cells. Mice treated with chlorine dioxide injections exhibited higher levels of immune cells in their blood and spleen compared to untreated mice. Additionally, elevated levels of cytokines, proteins that regulate immunity, were detected. These findings confirmed that chlorine dioxide prompts an immune reaction against the tumor.
In conclusion, this study demonstrated that chlorine dioxide has a dual effect. It causes tissue damage while also promoting healing. It effectively reduces tumor size by inducing cancer cell death and briefly activating the body's natural anti-cancer defenses. However, the immune-boosting properties of chlorine dioxide are short-lived, highlighting the need for further research to understand its effects and how to prolong its efficacy. These findings suggest that chlorine dioxide or a similar compound may hold potential for cancer treatment, provided scientists can overcome the transient nature of its immune-boosting properties.
IV. Research Conclusion
Our research has uncovered the promising versatility of chlorine dioxide as a potential therapy for cancer. Chlorine dioxide shares similarities with ROS, particularly in its ability to promote tissue regeneration. This makes it a promising candidate for enhancing wound healing in cancer treatment, as tumors can be seen as wounds that struggle to heal. By leveraging chlorine dioxide's regenerative properties, we may be able to improve patient recovery during cancer treatment.
Chlorine dioxide therapy offers several advantages over traditional cancer treatments. It not only reduces the complications and risks associated with the disease but also provides a safer and more effective option. Our proposed method of directly injecting chlorine dioxide into the tumor site allows for precise tumor destruction without encountering resistance, while simultaneously boosting the body's anti-cancer immune response. This targeted approach spares healthy tissue and takes advantage of chlorine dioxide's healing potential after tumor removal, aiming to enhance treatment outcomes.
The field of oncology is currently undergoing a transformation, thanks to immune checkpoint inhibitors. Ongoing clinical trials are exploring strategies such as intratumoral delivery and tumor-targeted compounds, which have shown promise in improving the local concentration of drugs and amplifying the effectiveness of immunotherapies. As new technologies emerge, the intratumoral administration of chlorine dioxide emerges as a viable, efficient, and patient-friendly approach to cancer treatment. This method has the potential to extend patient lifespans and alleviate the burden of treatment, revolutionizing cancer management into a more
chronic illness-like approach (Figure 14).
To fully harness the potential of chlorine dioxide in cancer treatment, continued research is crucial. We need to refine the protocols for administering chlorine dioxide, determine optimal dosages, explore its compatibility with other treatments, and gain a comprehensive understanding of its effects on tumor tissue—both in terms of regeneration and destruction—as well as its ability to stimulate a systemic anti-cancer immune response. The ongoing investigation into chlorine dioxide highlights its potential as a significant tool in cancer therapy, paving the way for improved patient care and clinical outcomes.
In line with the previous section, we need to consider five key dimensions when evaluating an ideal cancer treatment approach: convenience, safety, inhibition rate, drug resistance, and treatment sustainability. Based on the information provided in the table above, it is clear that intratumoral injection of chlorine dioxide for cancer treatment performs exceptionally well in all five aspects, establishing it as an optimal approach for treating cancer (Table 2).
16.3 Cancer Treatment Protocol
The intratumoral injection method is not very convenient, as it requires specialized equipment and facilities for preparation, and the administration of the injection should be carried out by qualified healthcare professionals. It is crucial to understand that currently, chlorine dioxide injection has not been approved as a new drug by any country. Therefore, within the existing medical system, no one, including myself, can utilize chlorine dioxide injection for treating individuals, unless they are conducting daring self-experiments. This treatment protocol should only be seen as a potential design for the future, and it should not serve as a foundation for treatment by anyone.
Standard Cancer Treatment Protocol:
A. Preparation of Chlorine Dioxide Injection:
Prepare an injection containing chlorine dioxide under Good Manufacturing Practice (GMP) conditions, with concentrations of 8mg/mL and 15mg/mL.
B. Treatment of Cancer with Chlorine Dioxide Injection:
If the injection has obtained approval from regulatory authorities, directly inject the chlorine dioxide injection into the tumor, following the principle of delivering a dose not exceeding half the volume of the tumor. If there are multiple tumors, it is advisable to inject the larger tumors whenever possible.
In exceptional circumstances, a self-experimentation protocol for cancer treatment may be available:
A. Preparation of Chlorine Dioxide Injection:
(1) Weigh 200 grams of sodium chlorite solid (powder, 80% purity, with the remaining 20% being sodium chloride) and add 800 milliliters of deionized water (or distilled water). Heat the mixture to around 50 degrees Celsius until all the solid has dissolved, then cool it to room temperature. This will result in a 16% sodium chlorite solution.
(1) Weigh 400 grams of citric acid solid (analytical grade, 99.9% purity) and add 600 milliliters of deionized water (or distilled water). Heat the mixture to around 50 degrees Celsius until all the solid has dissolved, resulting in a 20% citric acid solution.
(2) To produce a pure chlorine dioxide injection by absorbing chlorine dioxide through natural evaporation, follow these steps: Prepare a small open glass cup (e.g., 30-milliliter capacity) and a larger sealable glass cup (e.g., 300-milliliter capacity). Pre-fill the larger cup with approximately 30 milliliters of distilled water. Then, take 10 milliliters of each solution (sodium chlorite and citric acid) and mix them in the small glass cup. Quickly place the small cup into the larger cup and seal it tightly. Store the cups in a household refrigerator. After approximately 12 hours, the liquid in the larger cup will contain the desired chlorine dioxide injection (with a concentration of approximately 3-15mg/mL).
B. Storage of Chlorine Dioxide Injection:
Since chlorine dioxide easily evaporates from water, it is generally recommended to prepare the injection on-site and use it immediately. However, the preparation of chlorine dioxide-only injection is more complex. If a larger quantity needs to be prepared and stored for an extended period, it is recommended to store it in a glass bottle in a refrigerator at 2-8 degrees Celsius.
C. Method of Administration for Cancer Treatment:
Fill a syringe with the prepared injection and administer it intratumorally at the affected site. The principle of dosage control is not to exceed half the total volume of the tumor. During self-experimentation, it is generally not possible to seek the assistance of a doctor, so only patients with superficial tumors should attempt self-experimentation.







谢谢
Thank you! Grazie! Dankeschön! Gracias! Merci!
🙏
Well done. The oncologists will not like you, which is good.