5.1 Indications
5.1.1 Applicable for cancers in all parts of the pancreas, including periampullary, distal bile duct, second part of the duodenum, and uncinate process cancers.
5.1.2 Patients with normal blood count and coagulation profiles.
5.1.3 Metastatic pancreatic cancer, whether in single or multiple tumors.
5.1.4 Patients with recurrent pancreatic cancer post-surgery or where surgery was unsuccessful.
5.1.5 Patients who refuse surgery despite surgical indications.
5.1.6 When systemic chemotherapy fails.
5.2 Contraindications
5.2.1 Periampullary cancer with duodenal obstruction, preventing oral intake.
5.2.2 Severe jaundice, ascites, and cachexia.
5.2.3 PLT < 60×10⁹/L.
5.2.4 Pancreatic cancer with diabetes or active pulmonary tuberculosis.
5.2.5 KPS ≤ 40.
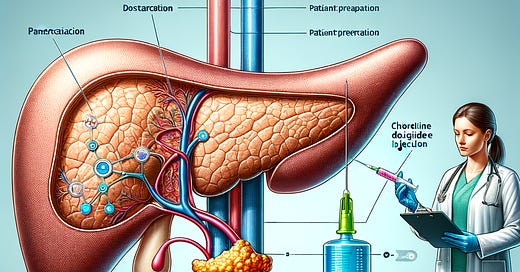
5.3 Pre-Treatment Preparation
5.3.1 Conduct necessary tests, including routine blood, urine, and stool tests, liver, kidney, and heart functions, and tumor markers like CA199, CA50, CEA, CA724.
5.3.2 Conduct a pre-treatment discussion and obtain informed consent.
5.3.3 Administer 0.1g buclizine, 1 KU antifibrinolytic drugs or 1.0g phenethylamine, and 4-8mg ondansetron intramuscularly 15 minutes before treatment to prevent pain, bleeding, and vomiting.
5.3.4 For CT-guided procedures, have the patient drink 500ml of 1%-2% gastrografin solution before treatment.
5.4 Needles and Auxiliary Equipment
5.4.1 Puncture needles: 23G×15.0 cm or 25G×9.0 cm.
5.4.2 Use ultrasound or CT scanners and syringes for guidance.
5.5 Procedure
5.5.1 Use ultrasound or CT to locate the puncture site and measure the distance to the tumor center.
5.5.2 Disinfect the area, wear sterile gloves, and apply sterile drapes.
5.5.3 Administer local anesthesia with 2% lidocaine, stabilize the site, insert the needle into the tumor center using imaging for guidance.
5.5.4 Remove the needle core, attach the syringe, and slowly inject the chlorine dioxide solution. For tumors ≤4 cm, use a single-point injection at 30% of the tumor volume; for larger tumors, use multiple points with each point receiving 30% of that section's volume.
5.5.5 After injection, briefly pause, remove the needle, cover the site, and observe the patient for 5-10 minutes before returning to the ward.
5.6 Post-Treatment Care
5.6.1 Monitor for fever, local pain, eating difficulties, or signs of peritonitis.
5.6.2 For fever, administer compound aminopyrine barbiturate and dexamethasone; for pain, use morphine or buclizine orally or inject as needed.
5.6.3 Recommend a liquid or semi-liquid diet for 1-3 days post-treatment to prevent duodenal obstruction; administer antibiotics for peritonitis.
5.6.4 Schedule subsequent treatments 5-7 days apart. Assess immune and tumor status via T lymphocyte subset testing and imaging before discharge or one week after treatment.
5.7 Clinical Experience
5.7.1 CT-guided injections are recommended as they provide a clear tumor view.
5.7.2 Ensure precise needle placement to avoid gastrointestinal puncture; strive for a single successful puncture.
5.7.3 If pain occurs during injection, administer additional lidocaine before proceeding.
5.7.4 Follow dosage calculations strictly, without unnecessary adjustments.
5.7.5 Manage acute inflammation post-injection as acute pancreatitis, potentially using octreotide.




The cds(PH 3 too low for inj.) has to made with an isotonic to cell solution that is PH balanced to 7 optimally.
DIY
1. 250ML of distilled water
2. add 2.5 grams of non ionized salt. celtic
3. add 1.5 grams of bobs red mill baking soda aluminum free. Strain in unbleached filter if needed.
4. ADD PHed saline water 100ml in CDS reation jar 500ml square sealed ball jar with rubber seal and latch to seal tight.
5. add 20ml of 22,4% sodium chlorite in shot jar. Then add 20ml of citric acid for gas reaction
6. seal jar to infuse gas for 24 hrs
7. repeat steps 5-6
8. check PH of solution before use. 7 -7.5PH
be very sanitary during prep in well ventilated area
This is all theory:)
Thank you for sharing this information. Could you tell me if this is using MMS or CDS?