Exploring Chlorine Dioxide as a Potential Therapy for Asthma
From Immune Misfires to a Radical New Hypothesis for Respiratory Health
Safety First: What We Already Know
In our clinical translation work, we have already accumulated 25 human cases and 3 veterinary cases with intratumoral chlorine dioxide (ClO₂) therapy. These experiences indicate that the therapy is safe and well-tolerated. Importantly, during treatment we consistently observed two key effects: selective destruction of pathological tissue (including fibrotic components) and clear reduction of local inflammation.
Beyond oncology, there is also a global experience base. Today, millions of people worldwide use chlorine dioxide daily in various forms—oral drops, topical application, even enemas. Remarkably, even the U.S. FDA quietly removed its previous warning on chlorine dioxide (see article).
Thus, while formal clinical trial data are still lacking for many indications, the accumulated evidence strongly suggests that the safety profile of ClO₂ is already well established. This foundation justifies further exploration of ClO₂ across multiple diseases where conventional treatments remain insufficient.
Part I. Understanding Asthma and the Limits of Current Therapies
Asthma is one of the most common chronic respiratory conditions in the world, affecting an estimated 235 million people according to the World Health Organization. While most prevalent in children and adolescents, asthma also increasingly affects adults and the elderly. The hallmark symptoms include:
Episodes of breathlessness, cough, and wheezing.
Chest tightness, particularly at night or in the early morning.
Variable and recurrent airway obstruction that can be reversible but often remains uncontrolled in severe cases.
At its core, asthma is driven by airway inflammation and hypersensitivity. The immune system of an asthmatic patient reacts to allergens, irritants, or pollutants with disproportionate responses, leading to swelling of the airway mucosa, bronchial smooth muscle contraction (bronchoconstriction), and mucus plugging. These processes narrow the airways, making breathing difficult and sometimes life-threatening.
Current Treatment Paradigms
Modern medicine has developed a layered approach to asthma management:
Inhaled corticosteroids (ICS) – cornerstone of long-term control, reducing inflammation.
Bronchodilators – short-acting β2-agonists (SABA) for acute relief, long-acting β2-agonists (LABA) for maintenance.
Leukotriene modifiers and biologics – targeting inflammatory mediators or immune pathways (e.g., anti-IgE, anti-IL-5, anti-IL-4R).
Emergency measures – systemic steroids, oxygen, hospitalization in severe cases.
Despite these interventions, asthma remains incurable. Even the most advanced biologics do not correct the immune mis-signaling that drives the disease.
Advances in Delivery Technology
One area of genuine progress has been inhalation delivery systems. In recent years, several European pharmaceutical innovators have developed advanced aerosol and dry powder inhalers capable of generating ultrafine particles that reach the distal small airways. This ensures more effective deposition and better patient adherence.
Yet while delivery has become more precise, the therapies themselves remain conventional—largely corticosteroids and bronchodilators. These drugs suppress inflammation and ease breathing but do not address the upstream immune dysfunction at the heart of asthma.
Part II. A New Perspective: Linking Asthma to Autoimmune Mechanisms
In my clinical work with chlorine dioxide (ClO₂), I have proposed a framework for treating autoimmune diseases by local delivery of this molecule. The principle is simple: autoimmune diseases arise when the immune system misidentifies normal tissue as foreign, launching chronic, destructive inflammatory attacks.
I have documented preliminary results in conditions such as alopecia areata (hair loss) and arthritis. In several patients, and in my own case, local ClO₂ application not only reduced symptoms but appeared to reset the immune system locally, leading to long-term remission or cure (see article on Autoimmune Diseases).
Asthma, while traditionally seen as an allergic disorder, shares key features with autoimmune disease:
Loss of tolerance – The immune system treats harmless triggers as dangerous.
Abnormal antigen recognition – Airways become hyperreactive to proteins or particulates.
Chronic inflammation – Immune cascades sustain airway swelling and remodeling.
From this perspective, asthma can be seen as a localized autoimmune-like condition of the airways. If ClO₂ can interrupt false immune signals and clear abnormal antigenic triggers in autoimmune disease, the same approach may apply to asthma.
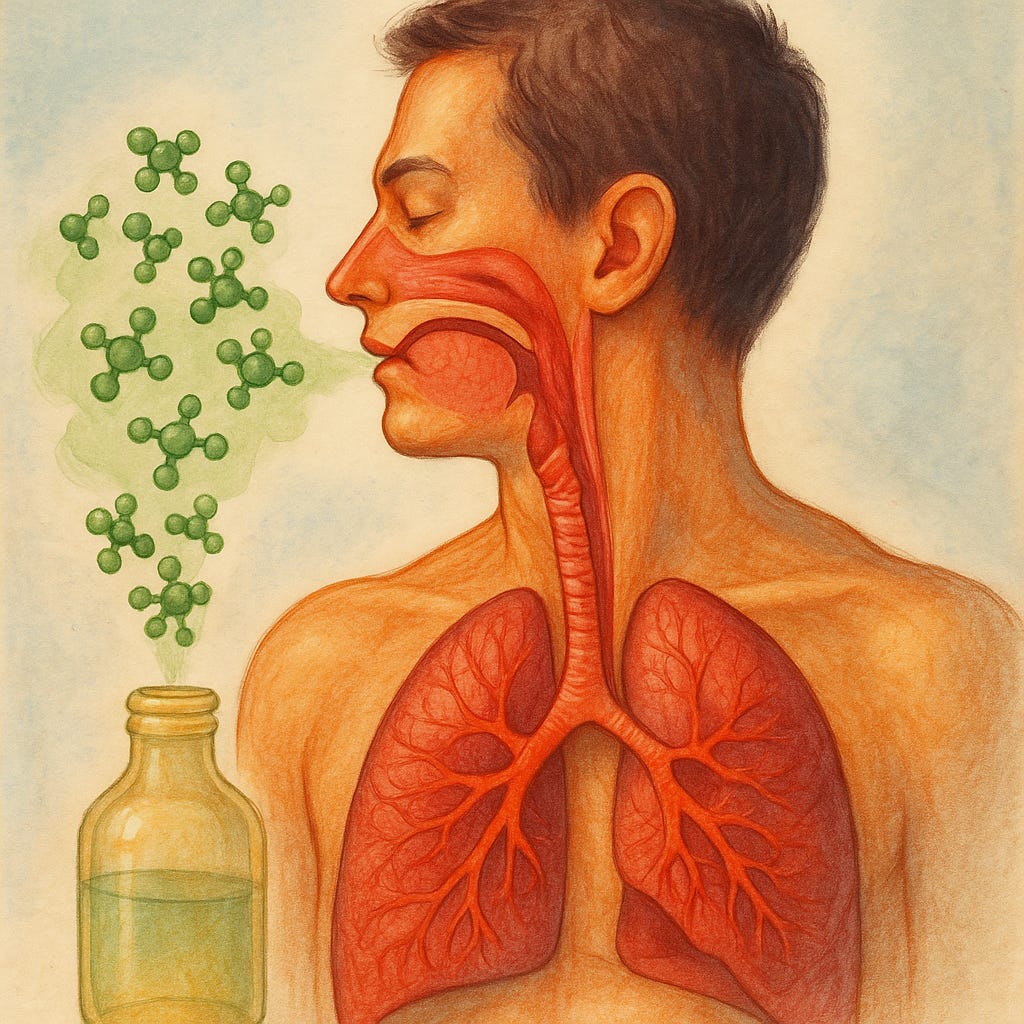
🔬 Mechanism Summary: How Chlorine Dioxide Could Work in Asthma
1. Antigen Clearance
Through selective oxidation, ClO₂ may remove abnormal proteins, allergen fragments, or inflammation-related antigens in the airways, reducing the “false targets” that trigger immune overreaction.
2. Immune Signal Modulation
ClO₂ mimics reactive oxygen species (ROS) and may act as a regulatory signal, perceived by the body as “immune saturation.” This could downregulate Th2 pathway activation, IgE release, and eosinophil infiltration.
3. Anti-inflammatory & Antimicrobial Action
By attenuating the release of inflammatory mediators from eosinophils and neutrophils, ClO₂ may reduce airway swelling; simultaneously, its antimicrobial properties could lower chronic infection triggers that worsen asthma.
4. Microenvironment Restoration
In chronic asthma, repeated inflammation leads to airway remodeling (smooth muscle hypertrophy, mucosal thickening, collagen deposition). Local ClO₂ exposure may help mitigate fibrosis and create conditions for epithelial cell regeneration.
Safety Note
While traditional toxicology studies set conservative safety thresholds for inhaled ClO₂ at below 0.1 ppm, our translational work with 25 human cases and 3 veterinary cases in intratumoral therapy, as well as anecdotal global use through oral, topical, and other routes, indicates a considerably wider safety margin. Exploratory inhalation exposures up to 10 ppm may still be well tolerated, provided that administration is intermittent, locally titrated by patient tolerance (stopping at the first sign of irritation), and closely monitored.
👉 Paid Subscribers Section Begins
The next part of this essay explores a potential therapeutic design for asthma using chlorine dioxide inhalation, building upon lessons from cancer therapy, autoimmune disease, and pulmonary fibrosis.
To access the proposed ClO₂ preparation approach, please refer to my book:
📖 The Chlorine Dioxide Miracle – Safeguarding Health with Safe and Effective Applications
In particular, the chapter on Dry Eye Syndrome provides detailed guidance on preparation and application of low-dose ClO₂ in mucosal tissues, which can serve as a practical reference for asthma-related exploration.
Keep reading with a 7-day free trial
Subscribe to Xuewu Liu’s Substack to keep reading this post and get 7 days of free access to the full post archives.